What are cysts, anyway?
As we wrap up PCOS awareness month, I thought I’d take a moment to summarize some of the questions and comments I’ve been answering online and in my private practice about the type of cysts associated with PCOS, and to differentiate them from other types of ovarian cysts. Cysts can seem scary, especially when you don’t know what causes them, or what they are made out of, so let’s break it down!
But first let’s take a second to recap PCOS basics. PCOS is a condition that is diagnosed when a woman has 2 out of 3 of the following:
Irregular ovulation (oligo-ovulation): ovulation doesn’t happen every month
Cysts on the ovaries that are sometimes referred to as a “ring of pearls”
Hirsutism: signs and symptoms of too much testosterone, including hair growth on the chest, stomach or back, male pattern hair loss on the head and cystic acne on the chin or back.
The other key thing to remember about PCOS is that it is actually a metabolic condition with fertility ‘side effects,’ which means that people with PCOS should make sure that they are
having their insulin sensitivity markers (like glucose and hemoglobin A1c) monitored regularly. People with PCOS are at higher risk for developing type 2 diabetes. For a deeper dive into PCOS, please check out my book, Feed Your Fertility. You’ll find all kinds of info, including recipes and supplements recommended for managing this chronic condition.
Now, let’s dive into cysts!
What is a cyst?
By definition, a cyst is a spherical area in any organ in the body that contains tissue that is different from the organ itself. The center of a cyst is usually liquid or soft tissue, whereas solid tissue is referred to as a tumor.
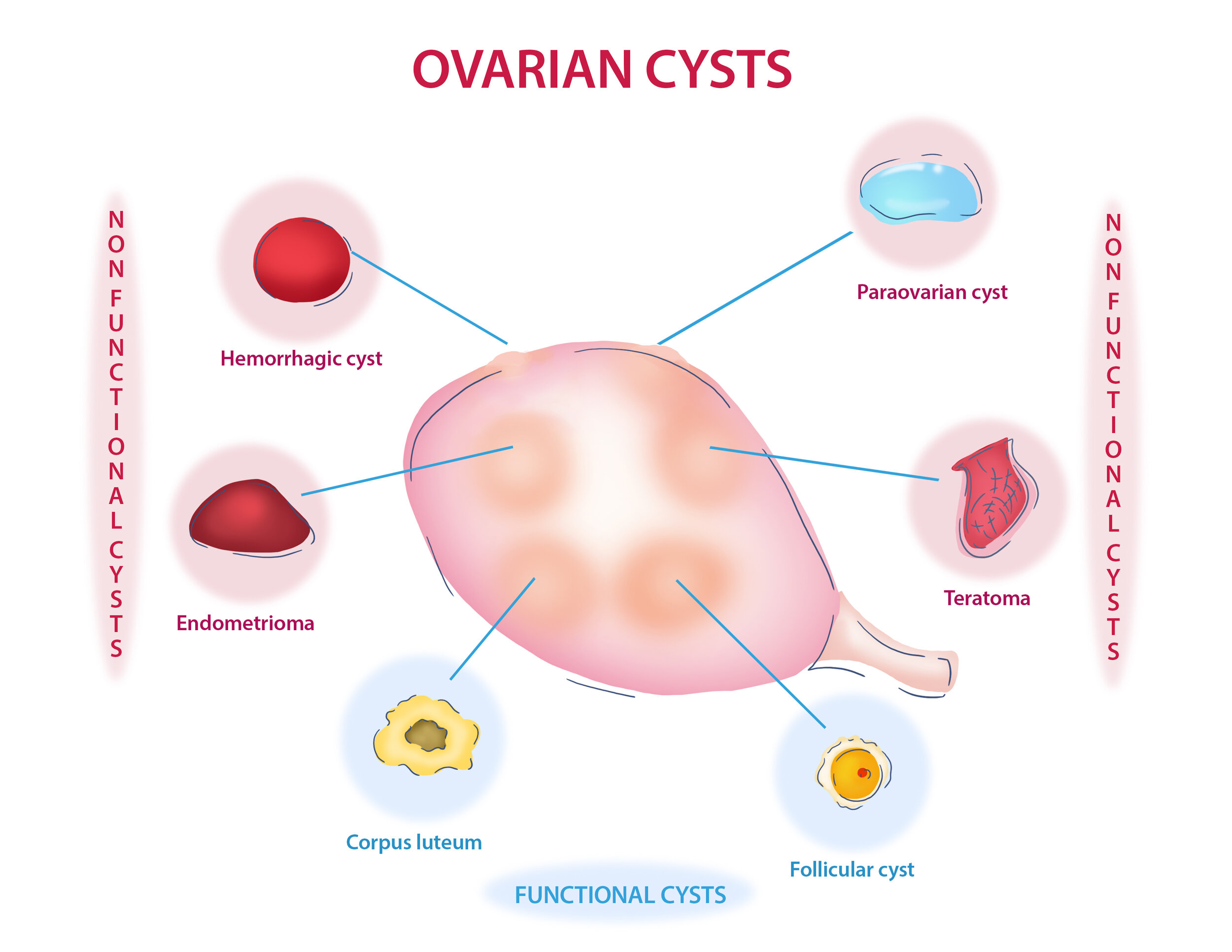
Within the ovaries, there are lots of different types of cysts, so let’s break down the most common ones. We’ll divide them into 2 categories, functional and non-functional.
Functional cysts:
Functional cysts are made up of follicles, which contain the eggs we ovulate mid-cycle each month. Follicles have a few jobs. In the first half of the cycle, their job is to make estrogen, which thickens the lining of the uterus, allows the follicle to grow, and sends signals to the brain when one is mature enough to ovulate. In turn, the brain sends the hormone LH down to the ovary, ovulation takes place, and the leftover ‘shell’ of the egg, called the corpus luteum, switches gears and starts producing progesterone. When that process doesn’t go according to plan, cysts can form. Here’s how:
Follicular cysts: In a normal cycle, follicle cysts are the eggs that grow and ovulate an egg. When ovulation doesn’t happen, they become what are known as functional cysts. These are the cysts that we see in folks with PCOS. In the most basic terms, they are follicles (eggs) that didn’t ovulate when they were supposed to, but instead keep growing and producing estrogen. This happens for a few reasons. First, it’s common for people with PCOS to have high testosterone levels. Too much testosterone in the ovaries causes follicles to stop growing before they mature, leaving a bunch of them in the ovaries making estrogen and with no way to ovulate. That in turn leads to high estrogen levels, or estrogen dominance. Too much estrogen + no ovulation= no period. Every now and then, a follicle will break through and ovulate, which is why people with PCOS sometimes will have really long cycles with occasional periods.
Corpus luteum cysts: Once the egg has ovulated, the outer shell of the follicle collapses and starts producing progesterone. If pregnancy occurs, the corpus luteum keeps on trucking through most of the first trimester, otherwise, it gives up the ghost after about 2 weeks, and your period begins. Corpus luteum cysts virtually always resolve on their own.
Non-functional cysts:
Non-functional cysts are composed of different types of tissue. What makes them non-functioning is that they don’t secrete hormones, but they can still complicate things if left untreated. Let’s look at a few of the most common non-functional cysts:
Hemorrhagic cysts: any cysts that bleed or appear to have blood vessels in them are considered a hemorrhagic cysts.
Endometriomas: these cysts are caused by endometriosis in the ovaries or other tissues. They produce a thick dark liquid inside their walls, which is why they are also sometimes called ‘chocolate cysts.’
Dermoid cysts: these are benign cysts, also called teratomas, which contain different types of tissues including hair, skin and nails. They usually form on the ovaries, testes or sacral area. They are benign, but removal is typically recommended because they can grow quite large if left untreated.
Paraovarian cysts: these are fluid filled sacs that grow near the ovaries or fallopian tubes. They usually resolve on their own.
Whether functional or not, cysts can cause complications with fertility or pain from rupture, unchecked growth, or bleeding. Cysts can be diagnosed via ultrasound, CT scans or MRI. All non-functional cysts should be monitored regularly based on your doctors recommendations.
When it comes to PCOS, it’s possible to make big improvements through natural means. Acupuncture, along with targeted herbs, supplements and dietary changes can play a huge role in increasing the frequency of ovulation, managing insulin resistance, and balancing androgen hormones like testosterone.
As always, please reach out with any questions. I’m more than happy to support you via either in-person care or virtual fertility coaching.